Rectal Prolapse
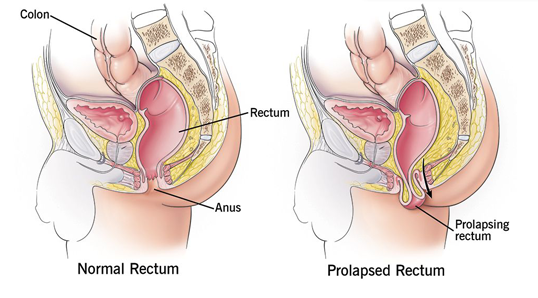
Rectal prolapse is where the rectum (the last section of the large intestine) protrudes through the anus. This can happen if the muscles and ligaments that support the rectum become weak or loose. Rectal prolapse often occurs in people with chronic (long-term) conditions such as Crohn’s disease, constipation, or cystic fibrosis. It can rarely be caused by childbirth, surgery, or an injury to the pelvis. Rectal prolapse is more common in older adults but can occur at any age. The most common symptom of rectal prolapse is the feeling that something is coming out of your anus. This may be accompanied by bleeding, mucus discharge, or fecal incontinence (leakage). Rectal prolapse can be painful and embarrassing, but it is treatable.
Signs and Symptoms
There is a constant feeling of discomfort in terms of emptying the bowels. The patient may complain of a sense of bulging in the anus. Rectal prolapse may also cause mucus discharge, anal pain, and difficulty passing stool. There may be itching and anal pain as well.
It is pretty common to mistake rectal prolapse for hemorrhoids. However, a proper physical examination by an experienced doctor can lead to a proper diagnosis.
Diagnosis and tests
A physical examination by a physician or a surgeon can help determine what they are affected by. Rectal nanometer gives us additional information about the prognosis of the patient post-treatment.
Treatment
Rectal prolapse is a chronic and progressive condition that requires medical attention at its earliest stage. The prognosis with early intervention, diet, and lifestyle management is much better than waiting for the situation to worsen. It is quite common after pregnancy due to the increased pressure on the veins from the growing uterus.
Rectal prolapse surgery (rectopexy) is done through the abdomen or the perineum (the region around the anus). The surgeon will discuss the options based on the size of the prolapse, age, general health condition, and technique used.
The procedure needs to be done under general anesthesia: however, it may also be done under a spinal block where only the lower half of your body is numbed, which means you will not feel any pain or discomfort during the procedure. Rectal prolapse surgery through the abdomen involves the surgeon making small incisions in your abdomen and pulling the rectum back into its place. In a laparoscopic rectopexy, even smaller incisions are made in the abdomen to enter the rectum. Surgical tools and a tiny camera enter through the incisions, and surgery is performed.
In the more commonly performed procedure, the surgeon pulls the rectum through the anus to remove a portion of the rectum and sigmoid and attaches the rest of the rectum to the large intestine (colon). Another method for shorter prolapses is done through the perineum (Delorme procedure). The rectum is shortened by removing the lining and folding the muscular layer.
Rectal prolapse repair can be done through a perineal approach, which is from the bottom side or abdomen. Depending on the severity, a mesh rectopexy is performed where the chances of recurrence are almost nil.
After a brief time in the hospital, your vitals and stability are checked. Once your bowel function is regained, and you are recovering, you will be discharged. The length of hospitalization will depend on the procedure performed and on your recovery. You will be asked to have clear fluids and gradually move to consume solid food with the help of stool softeners and laxatives. You can return to your normal activities in 4-6 weeks. Physical therapy sessions to exercise and use the pelvic floor muscles can also help.
